Widal test is a serological test that is used to detect the presence of antibodies against the typhoid-causing bacteria, Salmonella typhi, in the blood. It is a simple and inexpensive test that can be used to diagnose typhoid fever, but it has several limitations, including the potential for false-positive and false-negative results.
The Widal test is a simple and inexpensive test that can be performed in most laboratories. It is a useful tool for diagnosing typhoid fever, but it is not always accurate.
Introduction: Definition of the Widal test
The Widal test, named after Georges-Fernand Widal who developed it in 1896, is a serological test used to diagnose typhoid fever, a potentially life-threatening bacterial infection. It delves into the realm of the patient’s blood, searching for specific antibodies that act as telltale signs of the presence of the culprit bacteria, Salmonella typhi.
Think of the Widal test as a detective examining a crime scene. The blood is the scene, the antibodies are the clues, and the test is the meticulous analysis that reveals the identity of the suspect – Salmonella typhi. By uncovering the presence (or absence) of these antibodies, the Widal test sheds light on whether the patient is battling typhoid fever or not.
However, like any good detective story, there are twists and turns. Just as false alibis can mislead, the Widal test can sometimes lead to false-positive or false-negative results. Therefore, it’s crucial to understand the intricacies of the test, its limitations, and its role alongside other diagnostic tools in unmasking the true culprit – typhoid fever.
This introduction is just the starting point of our journey into the world of the Widal test. As we delve deeper, we’ll explore the intricate workings of the test, its interpretation, and its place in the fight against typhoid fever.
Principle of the Test
Here’s a breakdown of the principle behind the Widal test:
1. Agglutination: A Telltale Clump
The Widal test relies on a fundamental immunological phenomenon called agglutination. Imagine a microscopic dance party where antibodies are the guests and bacterial antigens are their dance partners. If they’re compatible, they’ll link arms and form visible clumps, like partygoers forming dance circles. This clumping or agglutination signals the presence of antibodies targeting specific antigens, indicating a possible infection.
2. The Antigen Lineup: O and H
In the Widal test, the suspects are two specific antigens from Salmonella typhi:
- O antigen: Found on the surface of the bacteria, like a fingerprint on a doorknob.
- H antigen: Found on the bacterial flagella, like propellers that help the bacteria move.
3. The Mixing and Matching: Serum and Antigens
The test involves a delicate dance between the patient’s blood serum and these antigens:
- Serum Collection: A small sample of the patient’s blood is drawn and the serum (the liquid part of the blood without cells) is separated.
- Antigen Introduction: The serum is carefully introduced to a sample of each antigen (O and H) on a slide or in a test tube.
4. The Verdict: Clump or No Clump
The dance begins:
- If antibodies against these antigens are present in the serum, they’ll eagerly link up with their corresponding antigens, forming visible clumps (agglutination). This is a positive Widal test, suggesting a possible typhoid fever infection.
- If no such antibodies are present, the dance floor remains empty, with no clumps forming. This is a negative Widal test, suggesting typhoid fever is less likely.
5. The Titer Twist: Measuring Antibody Levels
The test can also measure the strength of the antibody response, known as the titer. Higher titers generally indicate a stronger immune response to Salmonella typhi. However, interpreting titers requires careful consideration of other factors, which we’ll explore in later sections.
Procedure: Slide agglutination test
1. Preparing the Slide:
- A clean glass slide is taken, and its surface is divided into two or three sections, each marked for a different antigen (O, H, or both).
- A small drop of each antigen suspension is carefully placed onto its designated section.
2. Adding the Patient’s Serum:
- A drop of the patient’s serum is gently added next to each antigen drop, ensuring they don’t mix prematurely.
- A sterile wooden applicator stick or toothpick is used to mix the serum and antigen drops thoroughly.
3. Observing the Dance:
- The slide is gently tilted back and forth for about a minute, allowing the serum and antigens to interact.
- The mixture is observed closely, either with the naked eye or under a microscope, for any signs of agglutination (clumping).
4. Interpreting the Clumps:
- Positive agglutination: If visible clumps form, it indicates the presence of antibodies against the specific antigen, suggesting a possible typhoid fever infection.
- No agglutination: If no clumps form, it suggests the absence of these antibodies, making typhoid fever less likely.
5. Recording the Results:
- The presence or absence of agglutination for each antigen is recorded, along with any specific observations.
- If agglutination is observed, a semi-quantitative assessment of the agglutination strength (titer) may be performed using serial dilutions of the serum.
Key Points:
- The slide agglutination test is a rapid and relatively simple method for performing the Widal test.
- It’s often used as a screening test, but results should be interpreted with caution and considered alongside other clinical findings.
- The test is less sensitive than the tube agglutination method, meaning it may miss some cases of typhoid fever.
- It’s crucial to follow proper laboratory techniques and quality control measures to ensure accurate results.
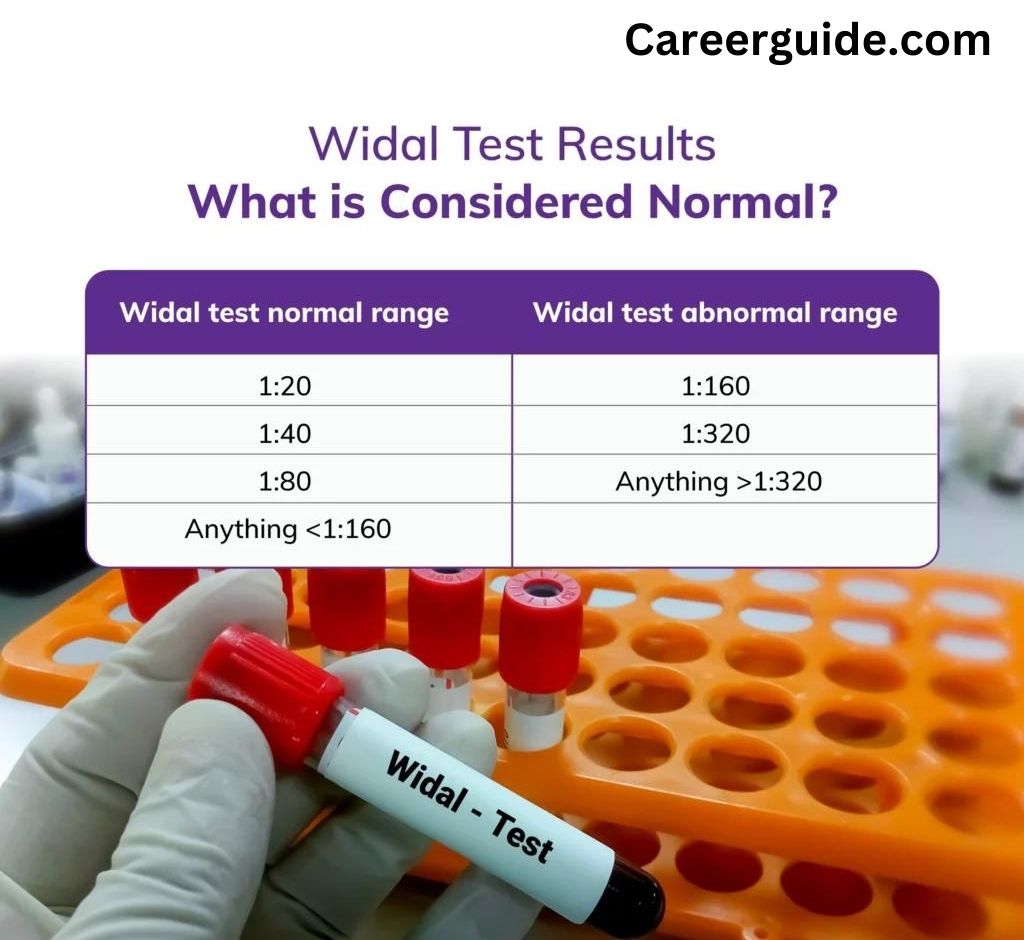
Interpretation of Results
1. Positive Widal Test:
- Agglutination observed: Clumps have formed on the slide or in the test tube, indicating the presence of antibodies against O and/or H antigens of Salmonella typhi.
- But hold your verdict! A positive test doesn’t automatically confirm typhoid fever. Consider these factors:
- Titers: The strength of agglutination (titer) is measured. Higher titers generally suggest a more active immune response, but they can also be influenced by previous infections or vaccinations.
- Timing: The test’s sensitivity is highest in the later stages of infection (around 10-14 days after onset). Early in the course, a negative test doesn’t rule out typhoid fever.
- Past Exposure: Past exposure to Salmonella typhi or vaccination can lead to lingering antibodies, causing false-positive results.
- Cross-Reactivity: Other bacteria, like Salmonella paratyphi or malaria, can sometimes trigger cross-reactions, mimicking a positive Widal test.
2. Negative Widal Test:
- No agglutination: No clumps have formed, suggesting an absence of antibodies against Salmonella typhi antigens.
- But don’t dismiss typhoid just yet: A negative test doesn’t always exclude typhoid fever, especially in the early stages of infection when antibody levels might be low.
3. Titer Trends:
- Rising titers: A significant increase in titers between two tests performed a week apart can support a typhoid fever diagnosis.
- Falling titers: Declining titers after treatment can indicate a positive response to therapy.
4. The Final Verdict:
- The Widal test results must be considered within the context of the patient’s clinical symptoms, travel history, exposure risks, and other laboratory findings.
- It’s often used as a supportive tool, not a standalone diagnostic test.
- If typhoid fever is strongly suspected, confirmatory tests like blood culture or bone marrow culture are usually recommended.
Clinical Applications: Diagnosis of typhoid fever
The Widal test, although not without its limitations, plays a crucial role in diagnosing typhoid fever, a potentially life-threatening bacterial infection. Let’s delve into how this test serves as a detective, sniffing out the clues of Salmonella typhi:
1. Early Suspicion:
- When a patient presents with symptoms like fever, headache, abdominal pain, and constipation, typhoid fever becomes a suspect. The Widal test steps in as the initial investigation, offering a quick and affordable clue.
2. Antibody Detective:
- The test searches for specific antibodies in the patient’s blood, the silent witnesses left behind by Salmonella typhi. Presence of these antibodies (O and/or H) points towards their interaction with the bacteria, suggesting a possible typhoid infection.
3. Titer Tales:
- The quantity of these antibodies, known as the titer, provides additional information. High titers suggest a robust immune response, possibly indicating an active infection. However, interpreting titers requires caution, as past exposure or other infections can also elevate them.
4. A Piece of the Puzzle:
- The Widal test alone rarely seals the case. It’s used alongside other evidence like clinical symptoms, travel history, and additional tests like blood culture or bone marrow culture, which offer more definitive proof of Salmonella typhi presence.
5. Early Warning System:
- The Widal test’s advantage lies in its ability to detect typhoid fever even in the early stages, when other tests might remain inconclusive. This early suspicion allows for prompt initiation of treatment, crucial for preventing complications.
6. Limitations to Consider:
- False positives due to past infections, vaccinations, or cross-reactions with other bacteria can mislead the investigation. False negatives, especially early in the disease, can require confirmation through other tests.
7. A Global Player:
- The Widal test’s affordability and simplicity make it a valuable tool, especially in resource-limited settings where typhoid fever remains prevalent.
Limitations: False-positive and false-negative results
The Widal test, while a helpful tool in diagnosing typhoid fever, is not a perfect detective. Like any good mystery, there are twists and turns, and sometimes the Widal test can lead us down the wrong path with false-positive and false-negative results. Let’s unravel these false leads:
False Positives:
These are like the red herrings that throw suspicion on the wrong suspect. Factors contributing to false positives in the Widal test include:
- Past Infection or Vaccination: Even after recovering from typhoid fever or receiving the typhoid vaccine, antibodies can linger in the blood, leading to a positive test despite no current infection.
- Cross-reactivity: Other bacteria, like Salmonella paratyphi or even malaria, share similar antigens with Salmonella typhi. Antibodies against these can mistakenly react with the test antigens, mimicking a positive result.
- Chronic Conditions: Certain chronic diseases like HIV, rheumatoid arthritis, and leprosy can alter antibody levels, leading to false-positive Widal results.
False Negatives:
These are like the missing clues that can leave us questioning our suspicions. False negatives in the Widal test can occur due to:
- Early Stage of Infection: In the early stages of typhoid fever, antibody levels might still be low, making the test miss the culprit.
- Antibiotics: Starting antibiotics early can suppress antibody production, leading to a false negative test.
- Malnutrition or Immunodeficiency: Conditions that weaken the immune system can impair antibody production, potentially resulting in a false negative.
How to navigate these false leads?
- Interpretation Matters: Consider the clinical context, travel history, and other laboratory findings along with the Widal test result. A single positive or negative test is rarely conclusive.
- Titer Trends: Monitoring changes in titers over time can be more informative than a single test result. Rising titers might suggest active infection, while falling titers could indicate response to treatment.
- Confirmatory Tests: When suspicion of typhoid fever is high, even with a negative Widal test, confirmation by blood culture or bone marrow culture is crucial.
Alternative Tests
While the Widal test remains a familiar name in the realm of typhoid fever diagnosis, it’s crucial to recognize that it’s not the only detective on the case. Here’s a look at some alternative tests that can offer more definitive clues:
1. Blood Culture:
- The gold standard for diagnosing typhoid fever. It directly isolates the Salmonella typhi bacteria from the patient’s blood, providing irrefutable evidence of their presence.
- More sensitive than the Widal test, especially in the early stages of infection.
- However, it can take several days for the bacteria to grow in culture, delaying the diagnosis.
2. Bone Marrow Culture:
- An even more sensitive option than blood culture, especially in the first week of infection.
- Involves extracting a small sample of bone marrow (usually from the hip bone) and culturing it for Salmonella typhi.
- More invasive than blood culture, requiring specialized equipment and expertise.
3. Polymerase Chain Reaction (PCR):
- A rapid and specific molecular test that detects the DNA of Salmonella typhi in the patient’s blood, stool, or bone marrow.
- Highly accurate and can provide results within hours.
- Can be expensive and requires specialized laboratory equipment and skills.
4. Typhoid Rapid Diagnostic Tests (RDTs):
- Point-of-care tests that offer quick results (often within 15-30 minutes) using fingerprick blood samples.
- Detect specific antigens or antibodies associated with Salmonella typhi.
- Less sensitive than blood culture or PCR but useful for rapid screening in resource-limited settings.
Conclusion
The Widal test, with its rich history and widespread use, has played a significant role in the fight against typhoid fever. Yet, its journey is not without its twists and turns. While it shines as a quick and affordable tool for initial suspicion, limitations like false positives and negatives demand caution. To fully unveil the mystery of typhoid fever, other investigative methods like blood culture, PCR, and rapid diagnostic tests come into play, each offering unique strengths and challenges.
Ultimately, the successful diagnosis of typhoid fever lies not in relying solely on any single test, but in carefully interpreting a combination of evidence. The Widal test serves as a valuable piece of this puzzle, offering a preliminary glimpse into the patient’s immune response. However, it’s only by integrating its findings with clinical symptoms, travel history, and other tests that we can confidently identify the true culprit – Salmonella typhi – and pave the way for effective treatment.
As research continues and diagnostic tools evolve, the fight against typhoid fever will see further advancements. However, the Widal test’s legacy as a pioneer in this field remains undeniable. Remembered for its simplicity and accessibility, it has undoubtedly saved countless lives, reminding us that even in the realm of complex medical mysteries, sometimes the most basic tools can offer invaluable clues.
FAQ's?
- A positive Widal test indicates the presence of antibodies against Salmonella typhi in the patient’s blood. However, it doesn’t automatically confirm typhoid fever, as false-positive results can occur due to past infections, vaccinations, or cross-reactions with other bacteria.
- A negative Widal test suggests an absence of antibodies against Salmonella typhi. But it doesn’t rule out typhoid fever, especially in the early stages of infection when antibody levels might be low.
- The test’s sensitivity is highest in the later stages of infection (around 10-14 days after onset).
- False-positive results can occur due to past infections, vaccinations, cross-reactions, or chronic diseases.
- False-negative results can occur in early stages of infection, due to antibiotics, or in those with weakened immune systems.
- Sensitivity is relatively low compared to blood culture or PCR.